Cancer Care Reimagined: clinical pathways and digital transformation
In our recent webinar on Cancer Care Reimagined, guest speaker Tatjana Kolevska, MD, medical director of the Kaiser Permanente National Excellence in Cancer Care program, presented on the core principles of our cancer care program and our successful use of cancer care pathways.
The Integrated Health Care in Action webinar series continues monthly through June, and international health care leaders are invited to join. The Center for Total Health is hosting the sessions on their innovative virtual platform. Take a virtual tour of the Center.
Generally speaking, in the United States and other countries, too much health care spending is spent on low-value care. Overall areas of waste include unnecessary testing, overtreatment, inefficient allocation of resources, and pricing failures. In order to decrease spending on low-value cancer care, it’s essential to bring in care coordination and technology. The cancer care pathways described below improve patient experience and outcomes while bringing efficiencies that prevent waste.
What’s more, Kaiser Permanente’s integrated system allows us to take a personalized approach to population health. By coordinating preventative care and treatment for manageable chronic conditions (hypertension, diabetes, obesity, vaccines), we can ensure better health for all patients, regardless of cancer diagnosis.
A 360-degree approach
Kaiser Permanente’s comprehensive cancer care approach uses the core touchpoints of prevention (including relapse surveillance), diagnosis, and treatment. With more than 30 service lines working in harmony, care teams across our regions can treat over 150 types of cancer. How is this complex coordination possible? Core principles of the cancer care program include:
- Leveraging clinical expertise and experience across all medical groups and care teams
- Providing seamless end-to-end cancer care with coordinated systems and digital tools
- Improving patient experience and care coordination through digital transformation of care delivery
To illustrate how these principles are put into practice, Dr. Kolevska gave numerous examples, including:
- Sub-specialization supported by telemedicine ensures the optimal use of physician resources. Every oncologist chooses a primary and a secondary cancer type to focus on. Specialized referrals can be made accordingly.
- A care team member ensures that a patient’s cancer diagnostic testing is done on schedule, and the results are ready for the specialist consultation. The patient is spared unnecessary delays and the burden of navigating the system.
- Recent experience has shown that 90% of cancer care can be done virtually. Tele-consults (virtual visits) allow patients to be hundreds or thousands of miles away from specialists while receiving expert care. Patients have experienced that video visits are convenient and beneficial, and other family members can join virtually and discuss the care plan. Follow-up treatment can be provided locally under the oncologist’s direction (for example, by a local infusion nurse).
Case conferences, clinical pathways, and digital transformation
Kaiser Permanente experts take part in virtual, multi-disciplinary case conferences to discuss complex cases in detail and develop treatment pathways. Case conferences are made possible by Kaiser Permanente’s integrated system, where collaboration is key and we do only what is medically necessary for the patient.
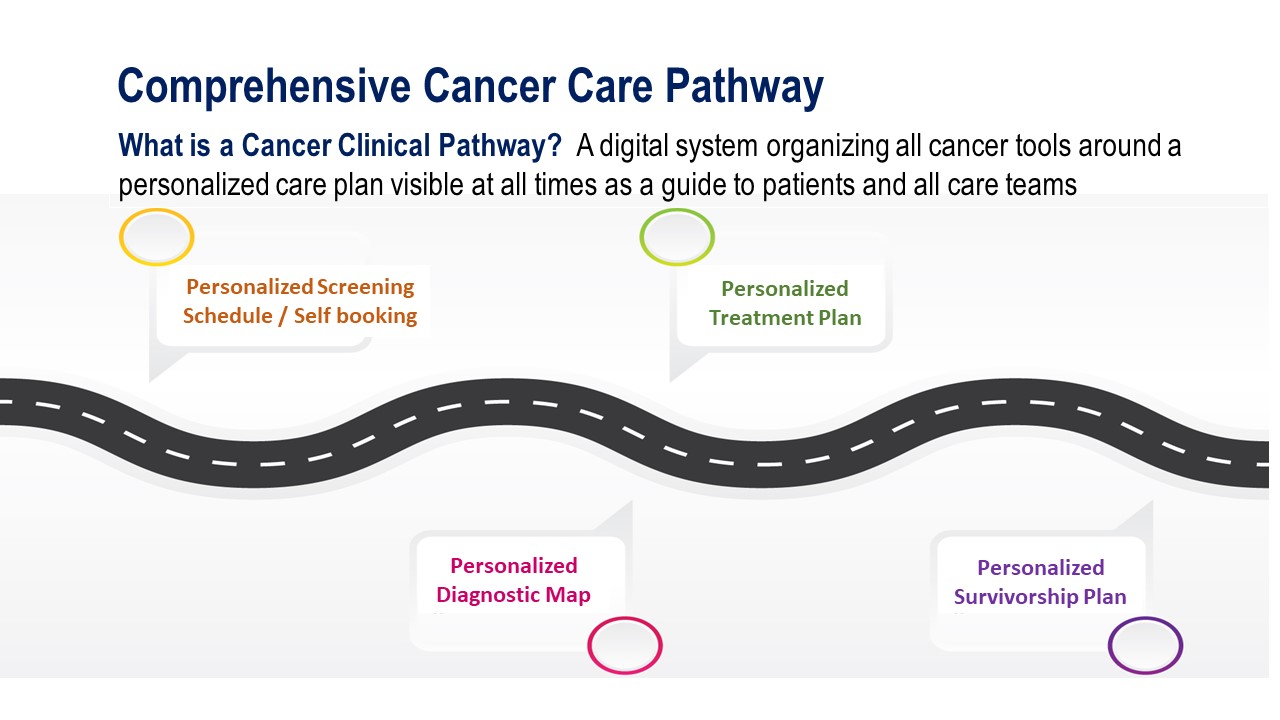
A clinical cancer pathway (see image above) is a digital system organizing all of the cancer tools around a personalized care plan that is visible at all times as a guide for patients and care teams. 94 evidence-based cancer care pathways have been developed and are updated quarterly. Care innovations that are developed in one area are piloted and tested before being spread throughout the organization. A clinical library is available to support care teams with the most up-to-date guidelines and research related to cancer treatments.
Digital transformation takes many other forms and brings other benefits. Within the electronic medical record that our clinical experts helped create and implement, we have created support tools for patient self-care, virtual navigation, and education. Studies show that with digital patient-reported symptom monitoring and follow-up during routine cancer treatment, outcomes and quality of life improve, and costs of emergency room visits and hospitalization decrease.
The future of cancer care
According to Dr. Kolevska, these are exciting times for cancer care leadership. When COVID-19 emerged, within one week of a mandatory shelter-in-place, virtual cancer care follow-up visits at Kaiser Permanente skyrocketed to 98%. Though that number has since decreased, many patients continue to prefer telemedicine when it’s medically appropriate. Now that many medical offices and exam rooms have gone virtual, the key to maintaining standards of excellence in cancer care is to use digital tools and cancer care pathways to proactively support patients in personalized population management. Technology allows us to follow our guiding principle of “the right care for the right patient at the right time.” Providing personalized care with the patient at the center – this is the essence of the integrated model.
For further reading, check out these research studies that were cited in the presentation:
- Physicians and cancer patients embrace virtual care in a pandemic
- Telehealth in Oncology during the Covid-19 Outbreak: Bringing the House Call Back Virtually
- Waste in the US Health Care System: Estimated Costs and Potential for Savings
Looking for more insights on the value of an integrated health system?
Join us for future sessions of Integrated Health Care in Action. View the webinar series description and registration.
Subscribe to our mailing list and stay current!
Health care leaders based outside the U.S. who are looking to drive transformation in their health system can subscribe for occasional news about Kaiser Permanente research and KP International programs. We do not share your data, and you can unsubscribe at any time.



